Eczema, a prevalent skin condition affecting people not only in Singapore but worldwide, can lead to discomfort and challenges that extend beyond the physical realm. It occurs when your skin struggles to retain moisture, resulting in dryness and heightened susceptibility to irritation. This dryness triggers the release of chemicals that intensify the irritation and provoke an irresistible urge to scratch. In this comprehensive guide, we delve into the intricacies of eczema, to equip you with a range of practical and holistic approaches for effective eczema treatment and management. Read on for insights on how you can regain control over your skin health and overall well-being.
6 Types of Eczema

There are several types of eczema, each with its distinct characteristics and specific triggers. In this section, we look into the most common types of eczema, shedding light on each type, as well as potential treatment options.
Atopic Dermatitis

Atopic dermatitis is the most common form of eczema, typically seen in children but can persist into adulthood. This type of eczema often has a genetic component and is associated with other allergic conditions, such as asthma and hay fever. It causes red, itchy rashes, most commonly on the face, hands, and behind the knees. Effective management of atopic dermatitis typically involves the application of moisturisers, topical corticosteroids, and the avoidance of known triggers that worsen the symptoms.
Contact Dermatitis
If you find yourself dealing with inflamed, itchy skin, or encountering a patch of thick, scaly skin caused by contact with certain substances, it’s possible that you are experiencing contact dermatitis.
There are two main types of contact dermatitis: Allergic contact dermatitis, a condition where the immune system responds to an irritant, such as latex or metals, resulting in skin reactions. On the other hand, irritant contact dermatitis arises when a chemical or other substance irritates the skin, leading to a range of dermatological symptoms.
Identification and avoidance of the specific irritants or allergens responsible for the condition is crucial for management. This often involves making lifestyle adjustments and employing protective measures. The application of topical treatments, like corticosteroids or barrier creams prescribed by a skin dermatologist, can also be instrumental in delivering relief by alleviating symptoms and establishing a shield against further skin irritation.
Stasis Dermatitis
Stasis dermatitis frequently affects individuals dealing with circulatory problems, primarily linked to conditions like varicose veins. This condition typically gives rise to rashes on the lower legs, presenting with noticeable symptoms such as swelling, redness, and skin scaling. Stasis dermatitis stems from compromised blood circulation in the lower extremities, often due to venous insufficiency, intensifying the risk factors for this skin issue.
Stasis dermatitis management involves using compression stockings and topical treatments to alleviate symptoms and prevent complications. It’s imperative to address this condition promptly, as untreated stasis dermatitis can lead to more severe complications.
Dyshidrotic Eczema
Dyshidrotic eczema, also referred to as pompholyx eczema, typically emerges in individuals under the age of 40. This condition primarily targets the hands and feet, appearing as small, itchy blisters on the palms and soles. In some instances, these blisters can grow in size and become filled with clear fluid. If left untreated, the blisters may become infected, leading to pain and swelling.
Individuals who frequently handle certain chemicals or have prolonged exposure to water are at a higher risk of developing dyshidrotic eczema. Emotional stress and weather changes also serve as potential triggers for this condition. Treatment may involve topical steroids, antihistamines, and efforts to avoid potential triggers.
Seborrheic Dermatitis
Seborrheic dermatitis is commonly known as dandruff when it affects the scalp. However, it can also appear on other parts of the body with an abundance of sebaceous glands, such as the face, chest, and back. This type of eczema is often associated with the overgrowth of yeast on the skin, and it can cause redness, scaling, and sometimes itching. To effectively manage seborrheic dermatitis, specially formulated shampoos and topical antifungal agents are often recommended. These treatments not only alleviate the symptoms but also help restore the skin’s natural balance, preventing the recurrence of this bothersome condition.
Neurodermatitis
Neurodermatitis, also known as lichen simplex chronicus, is characterised by thick, scaly patches of skin that result from persistent scratching or rubbing. The primary cause is psychological stress or anxiety, which can lead to a vicious cycle of itching and scratching. The condition often occurs in areas such as the neck, wrist, or ankle. Managing neurodermatitis requires addressing the underlying psychological triggers and finding healthier ways to cope with stress.
Causes of Eczema
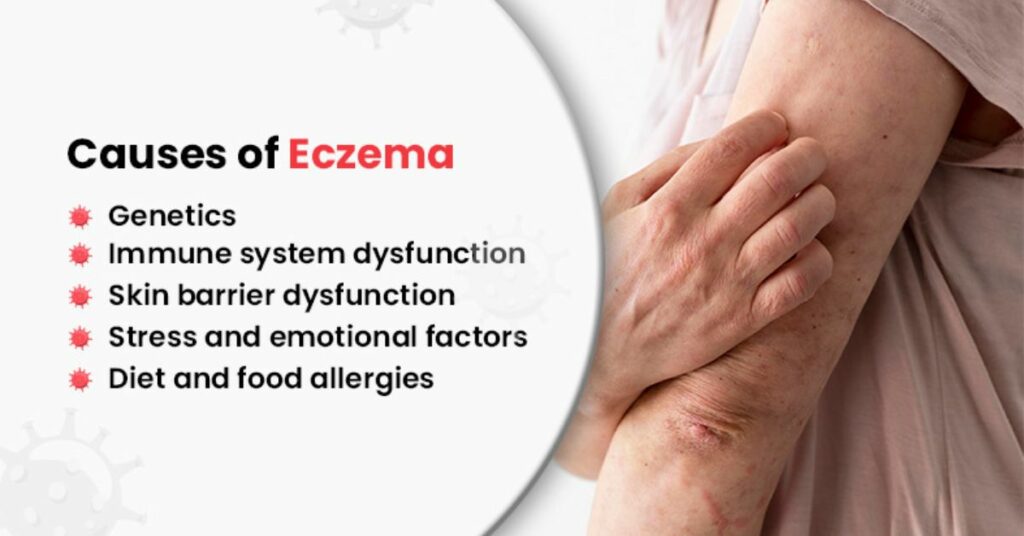
While the exact causes of eczema remain a subject of ongoing research, it is widely accepted that eczema is influenced by genetic, environmental, and immunological factors. Here, we look at these factors and how they interact to contribute to the development of eczema.
Genetics
Eczema often runs in families, which strongly suggests a genetic component. Individuals with a family history of eczema, asthma, or hay fever are more likely to develop the condition themselves. Researchers have identified specific genes that are associated with eczema, which influence skin barrier function, immune response, and inflammation. That said, while genetics play a role, they are just one piece of the puzzle, as not everyone with a genetic predisposition will develop eczema.
Immune System Dysfunction
In individuals with eczema, the immune system tends to overreact to environmental triggers. This heightened reactivity results in inflammation, characterised by the typical red and itchy skin symptoms. Exposure to allergens, such as dust mites, pet dander, pollen, and mould, can elicit an immune response in people with eczema. Irritants like harsh soaps, detergents, and certain fabrics can also exacerbate symptoms.
Skin Barrier Dysfunction
The human skin barrier serves as the outermost layer of our skin, comprising skin cells and specialised immune cells, working as a vital protective shield. It is responsible for recognising and repelling invading organisms and substances, akin to a protective wall. However, in individuals with eczema, this skin barrier’s functionality is compromised and may become “leaky” due to several factors.
One significant factor is the genetic variation in the filaggrin gene, responsible for encoding a key protein called filaggrin. Filaggrin plays a pivotal role in binding keratin filaments together, ensuring the structural integrity and flatness of skin cells. In cases where filaggrin is insufficient, skin cells lose moisture, contract, and form gaps between them, effectively creating “holes” in the skin’s defensive wall. This moisture loss leads to dry and itchy skin, encouraging scratching or rubbing, further weakening the skin barrier. Inadequate filaggrin production can also disrupt the skin’s pH balance, fostering abnormal bacterial growth that triggers immune responses such as inflammation.
Another essential element of the skin barrier is lipids. For those with eczema, these lipids may have a slightly different composition and contain reduced ceramide levels, a crucial component for retaining moisture.
Stress and Emotional Factors
Stress, anxiety, and emotional factors can worsen eczema symptoms. While not a direct cause, stress can weaken the immune system, making individuals more susceptible to flare-ups. Emotional stress may also lead to behaviours like scratching, which can worsen skin damage and inflammation. Hence, it’s essential for individuals with eczema to manage stress through relaxation techniques and seeking emotional support.
Diet and Food Allergies
Diet can be a contributing factor in certain instances of eczema, primarily among children. Specific food items, such as dairy, eggs, nuts, and soy, have been observed to initiate or intensify eczema symptoms in some individuals. Recognising and steering clear of these particular triggers can aid in eczema management.
Learn more: Misconceptions of Eczema in Singapore | Thomson Specialist Skin
4 tips for better management of eczema
Although a cure for eczema remains elusive, numerous approaches can be employed to efficiently handle its symptoms and enhance your overall quality of life. Read on as we share valuable suggestions for more effective eczema management.
Maintain Proper Hygiene

Maintaining proper hygiene is vital for eczema management. Choose a mild, unscented cleanser or soap, as harsh products and hot water can remove natural skin oils, increasing dryness and irritation. Opt for lukewarm water, as it’s gentler on your skin, and remember to keep baths or showers brief, lasting 10-15 minutes. Afterwards, adopt the practice of gently patting your skin dry with a soft towel instead of vigorous rubbing. These measures collectively contribute to a more effective eczema management routine, ensuring your skin remains well-hydrated and less prone to irritation.
Wear Breathable Fabrics
Selecting appropriate clothing is integral to effective eczema management. Choose soft, breathable materials such as cotton, which allows your skin to breathe and reduces the risk of irritation. Avoid scratchy or rough fabrics like wool, as they can exacerbate itching and discomfort. Additionally, opt for loose-fitting clothing, as it minimises friction on your skin, reducing the risk of irritation.
Moisturise Regularly

One of the most critical aspects of eczema management is keeping your skin well-hydrated. The key is to incorporate a high-quality, fragrance-free moisturiser into your daily routine to help seal in moisture. This practice is vital both immediately after bathing and consistently throughout the day.
Moisturisers serve a dual purpose, not only replenishing lost moisture but also forming a protective shield on your skin’s surface. This shield acts as a safeguard against excessive drying, subsequently diminishing the chances of eczema flaring up. In essence, the consistent use of moisturisers bolsters your skin’s resilience, fostering a more comfortable, healthier complexion and mitigating the discomfort often associated with eczema.
Consult a Dermatologist
Seeking the expertise of a dermatologist is a pivotal step in your journey to effectively manage eczema. These medical professionals specialise in the diagnosis and treatment of skin conditions, ensuring you receive personalised and expert guidance.
When you consult a dermatologist, they will conduct a comprehensive evaluation of your condition, taking into account your medical history, lifestyle, and specific triggers. This detailed assessment allows them to tailor recommendations and eczema treatments to your unique needs. Some examples include the use of advanced topical treatments, such as corticosteroids or immunomodulators, which can effectively manage inflammation and itching. They may also recommend phototherapy, which involves controlled exposure to UVB light to alleviate eczema symptoms. Moreover, they can offer valuable advice on lifestyle modifications, dietary considerations, and stress management techniques, all of which play a critical role in eczema management.
Questions You May Have
We conclude this guide with a few common questions you may have regarding treating eczema.
Is Eczema Contagious?
No, eczema is not a contagious condition and is not the result of bacteria, viruses, or other pathogens. Thus, it is a non-infectious condition that cannot be transmitted to others through contact.
What are Some Common Symptoms of Eczema?
Eczema symptoms can vary from one person to another. However, common symptoms of eczema often include red, itchy skin, dryness, inflammation, and the formation of rashes or patches.
Are There Specific Dietary Restrictions for Individuals With Eczema?
Individuals with eczema often benefit from avoiding or reducing certain foods that can trigger or worsen their symptoms. Common culprits include dairy products, eggs, nuts, seeds, wheat, soy, fish, and processed foods, as well as artificial additives and preservatives. However, food triggers can vary from person to person, so it’s essential for those with eczema to work with healthcare professionals to identify specific problem foods to aid in managing the condition.
What are Some Examples of Eczema Treatment?
Eczema can be treated with moisturisers, topical corticosteroids, antihistamines, and other medications prescribed by a healthcare professional. Lifestyle changes and avoiding triggers are also essential for management.
Conclusion
Eczema is a challenging skin condition that can significantly impact an individual’s quality of life. However, with these strategies provided, you can effectively manage and relieve its symptoms. Keep in mind that there’s no one-size-fits-all solution for dealing with eczema, so it might take some time to find the right treatments and lifestyle changes that work for you. The key is to stay patient and positive, and work closely with healthcare professionals to create a plan that fits your needs.
Ready to take control of eczema with effective management techniques? At Thomson Specialist Skin Centre, we offer a range of treatments, including eczema treatments, laser treatments for the face and body, as well as acne treatments. Contact our team of dermatologists today to learn more and start your journey towards healthier skin.

